News
Notice of Publication of Article on Results of Late Phase II Study of Novel Coronavirus Lung Injury
We are pleased to announce that the results of a late phase II study of our PAI-1 inhibitor RS5614 for novel coronavirus lung injury have been published in the scientific journal “Scientific Reports”.
Hirai T, Asano K, Ito I, Miyazaki Y, Sugiura H, Agirbasli M, Kobayashi S, Kobayashi M, Shimada D, Natsume I, Kawasaki T, Ohba T, Tajiri S, Sakamaki F, Mineshita M, Takihara T, Sekiya K, Tomii K, Tomioka H, Kita H, Nishizaka Y, Fukui M, Miyata T, Harigae H Mineshita M, Takihara T, Sekiya K, Tomii K, Tomioka H, Kita H, Nishizaka Y, Fukui M, Miyata T, Harigae H.
A randomized double-blind placebo-controlled trial of an inhibitor of plasminogen activator inhibitor-1 (TM5614*1) in mild to moderate COVID-19. Scientific Reports. 2024 online.(http://doi.org/10.1038/s41598-023-50445-1)
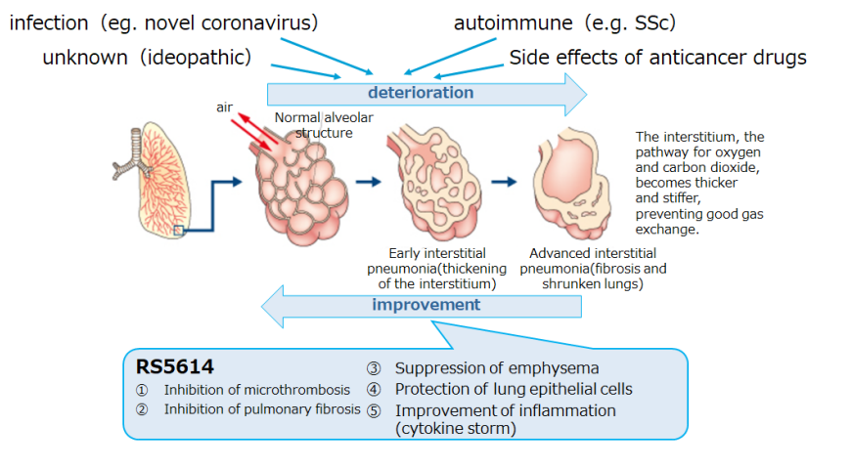
RS5614, a PAI-1 inhibitor, suppresses inflammation, fibrosis, and vascular damage in the lung, and thus may be effective against interstitial lung diseases by various causes, including novel coronavirus.
An early phase II investigator-initiated clinical trial was conducted in collaboration with seven medical institutions in Japan to explore the efficacy and safety of RS5614 in patients with novel coronavirus pneumonia, and the results showed that the primary endpoint of “deterioration requiring ventilator management” was “none” in all patients, and that there were no serious side effects for which a causal relationship with the investigational drug could not be denied, suggesting that RS5614 is effective and safe in preventing the serious illnesses. Based on the results of the early phase II study, a placebo-controlled late phase II investigator-initiated clinical trial was conducted in 100 patients with novel coronavirus lung injury (moderate, hospitalized) in collaboration with 20 major medical institutions in Japan including Tohoku University, Kyoto University, Tokyo Medical and Dental University, Tokai University, as well as Istanbul Medeniyet University, Republic of Turkey. The trial began in June 2021 and was extended to October 2022 due to a period of sharp decline in the number of patients infected with novel coronavirus and a decrease in the number of eligible patients with new coronavirus lung injury (moderate, hospitalized) due to the emergence of the Omicron variant*2 (finally 75 patients enrolled). The clinical study report was completed in April 2023.
Although the primary efficacy endpoint, “the sum of oxygenation scale*3,” showed no statistically significant difference between the RS5614 group and the placebo group due to the small number of patients enrolled (n = 75), there was a reduction in worsening lung injury in the RS5614 group versus the placebo group among patients with moderate disease. In particular, there was a reduction in the need for oxygen therapy (prevention of severe disease) in patients of Moderate I*4 who had pneumonia and dyspnea on admission but did not require oxygen therapy. In addition, the proportion of patients who required oxygen was lower in the RS5614 group in the first 3-5 days after hospitalization, suggesting the effectiveness of RS5614 in the early treatment of patients. The RS5614 group also showed improvement in pneumonia imaging, unlike the placebo group. The incidence of side effects was similar between the RS5614 and placebo groups, confirming the safety of RS5614 in patients with novel coronavirus lung injury. We have prepared to start the next phase of the clinical trial as soon as the number of target pneumonia patients increases due to mutant strains, etc. The consultation with PMDA was already conducted on April 11, 2023.
As for development in other interstitial lung diseases, we have initiated a collaboration with the Department of Respiratory Medicine, Kyoto University Hospital, with a view to conducting clinical trials for acute exacerbations of idiopathic interstitial pneumonia*5 (December 23, 2022). We have also extended the agreement with Daiichi Sankyo Company, Limited with a view to conducting clinical trials to confirm the efficacy of RS5614 in the treatment of interstitial pneumonia arising from anticancer drug therapy, etc. (November 28, 2022). In addition, Renascience executed another collaboration agreement with Kyoto University and Daiichi Sankyo Company, Limited to conduct research and development in the area of lung injury (June 5, 2023). Furthermore, a placebo-controlled, double-blind, phase II investigator-initiated clinical trial to investigate the efficacy and safety of RS5614 for interstitial pneumonia associated with systemic scleroderma*6 was initiated in collaboration with 11 medical institutions in Japan including Tohoku University Hospital and The University of Tokyo Hospital, with funding from the Japan Agency for Medical Research and Development (October 19, 2023).
*1 TM5614
Clinical development number of RS5614 (PAI-1 inhibitor).
*2 Omicron variant
The Omicron variant is one of the mutant strains of the novel coronavirus (SARS-CoV-2). In Japan, the conventional strain first discovered in Wuhan, China, spread, followed by the alpha and then the delta variants. The Omicron variant caused the 6th, 7th, and 8th waves of epidemics in Japan, and many subvariants have been reported to date. Infections with the Omicron variants have been shown to carry a relatively low risk of hospitalization and severe illness compared to the delta variant.
*3 Sum of oxygenation scale
It is the sum of scores to evaluate oxygenation requiring oxygen administration therapy or ventilator management up to 14 days after the start of the clinical trial, and is an evaluation index established based on scientific and medical validity through consultation with respiratory specialists and the Pharmaceuticals and Medical Devices Agency (PMDA). The oxygenation status of the subjects was compared by assigning a score ranging from no oxygen (Point 0) to wearing the artificial ventilator ECMO (Point 5) (e.g., Point 2 for oxygen administration of 2L or more, but less than 5L), on a daily basis for a total of 14 days.
*4 Moderate I
It is defined in the Clinical Management of Patients with COVID-19: A guide for front-line healthcare workers, Version 9.0.
- Moderate I: Novel coronavirus infection, with blood oxygen levels between 93% and 96%, dyspnea and initial findings of pneumonia, but no respiratory failure and no oxygen administration therapy.
- Moderate II: Stage in which the blood oxygen level is less than 93%, respiratory failure is present, and oxygen administration therapy is required.
- Severe: Stage requiring intensive care or ventilator management
*5 Idiopathic interstitial pneumonia
There are various known causes of interstitial pneumonia, including connective tissue diseases (autoimmune diseases) such as rheumatoid arthritis and dermatomyositis; drugs such as anticancer agents; and special infectious diseases. Interstitial pneumonia for which no cause can be found after various detailed investigations is called “idiopathic interstitial pneumonia”.
*6 Systemic scleroderma
Systemic scleroderma (SSc) is a chronic, progressive autoimmune disease characterized by hardening of the skin and internal organs (called sclerosis). It is designated as an intractable disease, and more than 20,000 patients have been identified in Japan.